-
SUMMARY
-
Osteomyelitis in the pediatric population is most often the result of hematogenous seeding of bacteria to the metaphyseal region of bone.
-
Diagnosis is generally made with MRI studies to evaluate for bone marrow edema or subperiosteal abscess.
-
Treatment is nonoperative with antibiotics in the absence of an abscess. Surgical debridement is indicated in the presence of an abscess.
-
-
EPIDEMIOLOGY
-
Incidence
-
1 in 5000 children younger than 13 years old
-
-
Demographics
-
mean age 6.6 years
-
2.5 times more common in boys
-
more common in the first decade of life due to the rich metaphyseal blood supply and immature immune system
-
not uncommon in healthy children
-
-
Anatomic location
-
typically metaphyseal via hematogenous seeding
-
-
Risk factors
-
diabetes mellitus
-
hemoglobinopathy
-
juvenile rheumatoid arthritis
-
chronic renal disease
-
immune compromise
-
varicella infection
-
-
-
ETIOLOGY
-
Pathophysiology
-
mechanism
-
local trauma and bacteremia lead to increased susceptibility to bacterial seeding of the metaphysis
- history of trauma is reported in 30% of patients
- history of trauma is reported in 30% of patients
-
-
microbiology
-
Staph aureus
-
is the most common organism in all children
-
strains of community-acquired (CA) MRSA have genes encoding for Panton-Valentine leukocidin (PVL) cytotoxin
- PVL-positive strains are more associated with complex infections, multifocal infections, prolonged fever, abscess, DVT, and sepsis
- MRSA is associated with increased risk of DVT and septic emboli
-
-
Group B Strep
-
is most common organism in neonates
-
-
Kingella kingae
-
becoming more common in younger age groups
-
-
Pseudomonas
- is associated with direct puncture wounds to the foot
- is associated with direct puncture wounds to the foot
-
H. influenza
-
has become much less common with the advent of the Haemophilus influenza vaccine
-
-
Mycobacteria tuberculosis
-
children are more likely to have extrapulmonary involvement
-
biopsy with stains and culture for acid-fast bacilli is diagnostic
-
-
Salmonella
-
more common in sickle cell patients
-
-
-
pathoanatomy
-
acute osteomyelitis
-
most cases are hematogenous
-
initial bacteremia may occur from a skin lesion, infection, or even trauma from tooth brushing
-
microscopic activity
-
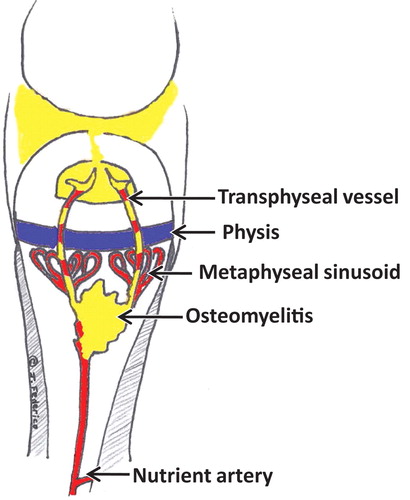
sluggish blood flow in metaphyseal capillaries due to sharp turns results in venous sinusoids which give bacteria time to lodge in this region
-
the low pH and low oxygen tension around the growth plate assist in the bacterial growth
-
infection occurs after the local bone defenses have been overwhelmed by bacteria
-
spread through bone occurs via Haversian and Volkmann canal systems
-
purulence develops in conjunction with osteoblast necrosis, osteoclast activation, the release of inflammatory mediators, and blood vessel thrombosis
-
-
macroscopic activity
- a subperiosteal abscess develops when the purulence breaks through the metaphyseal cortex
- septic arthritis develops when the purulence breaks through an intra-articular metaphyseal cortex (hip, shoulder, elbow, and ankle) (NOT KNEE)
- a subperiosteal abscess develops when the purulence breaks through the metaphyseal cortex
-
Infants <1 year of age can have infection spread across the growth plate via capillaries causing osteomyelitis in the epiphysis and septic arthritis
-
-
chronic osteomyelitis
-
periosteal elevation deprives the underlying cortical bone of blood supply leading to necrotic bone (sequestrum)
-
sequestrum
-
the necrotic bone which has become walled off from its blood supply and can present as a nidus for chronic osteomyelitis
-
-
-
an outer layer of new bone is formed by the periosteum (involucrum)
-
involucrum
- a layer of new bone growth outside existing bone seen in osteomyelitis
- a layer of new bone growth outside existing bone seen in osteomyelitis
-
- chronic abscesses may become surrounded by sclerotic bone and fibrous tissue leading to a Brodie's abscess
-
-
-
-
-
ANATOMY
-
Blood supply
-
the metaphyseal blood capillaries undergo sharp turns prior to entering venous sinusoids leading to turbulent flow and predisposition of bacterial deposition
-
-
-
CLASSIFICATION
-
Acute osteomyelitis
-
see pathoanatomy above
-
-
Subacute osteomyelitis
- uncommon infection with bone pain and radiographic changes without systemic symptoms
-
increased host resistance, decreased organism virulence, and/or prior antibiotic exposure
-
radiographic classification
-
types IA and IB show lucency
-
type II is a metaphyseal lesion with cortical bone loss
-
type III is a diaphyseal lesion
-
type IV shows onion skinning
-
type V is an epiphyseal lesion
-
type VI is a spinal lesion
-
- uncommon infection with bone pain and radiographic changes without systemic symptoms
-
Chronic osteomyelitis
-
see pathoanatomy above
-
-
-
PRESENTATION
-
History
-
limb pain
-
recent local infection or trauma
-
obtain immunization history regarding H. influenza
-
ask about prior antibiotic use, as it may mask symptoms
-
-
Symptoms
-
limp or refusal to bear weight
-
generally not toxic appearing
-
+/- fever
-
-
Physical exam
-
inspection & palpation
-
edematous, warm, swollen, tender limb
-
evaluate for point tenderness in pelvis, spine, or limbs
-
-
range of motion
-
restricted motion due to pain
-
-
-
-
IMAGING
-
Radiographs
-
recommended views
-
obtain AP and lateral of the suspected area
-
-
findings
- early films may be normal or show loss of soft tissue planes and soft tissue edema
-
new periosteal bone formation (5-7 days)
-
osteolysis (10-14 days)
-
late films (1-2 weeks) show metaphyseal rarefaction (reduction in metaphyseal bone density) or possible abscess
- early films may be normal or show loss of soft tissue planes and soft tissue edema
-
-
CT
-
indication
-
more helpful later in the disease course to demonstrate bone changes or abscesses
-
-
-
MRI
-
detects abscesses and early marrow and soft tissue edema
-
indications
- can assist with decision making when a poor clinical response to antibiotics or surgical drainage considered
- can assist with decision making when a poor clinical response to antibiotics or surgical drainage considered
-
views
-
T1 signal decreased
-
T1 with gadolinium signal increased
-
T2 signal increased
-
-
88% to 100% sensitivity, sensitivity increased by Gadolinium contrast
-
-
Bone scan
-
indications
-
nondiagnostic x-ray
-
need to localize pathology in infant or toddler with non-focal exam
-
-
technetium-99m can localize the focus of infection and show a multifocal infection
-
92% sensitivity
-
a cold bone scan may be associated with more aggressive infections
-
-
-
STUDIES
-
Serum labs
- WBC count
-
elevated in 25% of patients and correlates poorly with treatment response
-
-
C-reactive protein
-
elevated in 98% of patients with acute hematogenous osteomyelitis
-
becomes elevated within 6 hours
-
most sensitive to monitor therapeutic response
-
declines rapidly as the clinical picture improves
- CRP is the best indicator of early treatment success and normalizes within a week
-
failure of the C-reactive protein to decline after 48 to 72 hours of treatment should indicate that treatment may need to be altered
-
-
-
ESR
-
elevated in 90% of patients with osteomyelitis
-
rises rapidly and peaks in three to five days, but declines too slowly to guide treatment
-
less reliable in neonates and sickle cell patients
-
-
plasma procalcitonin
-
new serologic test that rises rapidly with a bacterial infection, but remains low in viral infections and other inflammatory situations
-
elevated in 58% of pediatric osteomyelitis cases
-
-
bone aspiration
-
helps establish a definitive diagnosis
-
50% to 70% of affected patients have positive cultures
-
-
blood culture
-
is positive only 30% to 50% of the time and will likely be negative soon after antibiotics are administered, even if treatment is not progressing satisfactorily
-
- WBC count
-
Aspiration
-
assists in diagnosis and management
-
helps guide antibiotic selection when organism identified (50% of the time)
-
proceed with surgical drainage if pus is aspirated
-
-
technique
-
large bore needle utilized to aspirate the subperiosteal and intraosseous spaces under fluoroscopic or CT-guidance
-
start antibiotics after aspiration
-
-
-
Biopsy and culture
-
consider when diagnosis not clear (i.e. subacute osteomyelitis) and need to rule out malignancy
-
-
-
TREATMENT
-
Nonoperative treatment
-
antibiotic therapy alone
-
indications
-
early disease with no subperiosteal abscess or abscess within the bone
-
surgery is not indicated if clinical improvement obtained within 48 hours
-
-
modalities
-
antibiotics
-
begin with empiric therapy
-
generally, nafcillin or oxacillin, unless high local prevalence of MRSA (then use clindamycin or vancomycin)
-
mechanism of action for vancomycin involves binding to the D-Ala D-Ala moiety in bacterial cell walls
-
if gram stain shows gram-negative bacilli - add a third generation cephalosporin
-
-
convert to organism-specific antibiotics if organism identified
-
mycobacterium tuberculosis
-
treatment for initial 1 year is multiagent antibiotics and rarely surgical debridement due to risk of chronic sinus formation
-
-
duration
-
typically treat with IV antibiotics for four to six weeks
-
controversial duration
-
-
- intravenous versus oral
-
often a case by case decision with input from infectious disease consultation
-
-
-
-
-
-
Operative treatment
-
surgical drainage, debridement, and antibiotic therapy
-
indications
- deep or subperiosteal abscess
- failure to respond to antibiotics
-
chronic infection
- deep or subperiosteal abscess
-
contraindications
- hemodynamic instability, as patients should be stabilized first - however sometimes operative treatment of the underlying infection helps stabilize the patient
- hemodynamic instability, as patients should be stabilized first - however sometimes operative treatment of the underlying infection helps stabilize the patient
-
example of institution algorithm treatment pathway
-
-
-
-
TECHNIQUE
-
Surgical drainage, debridement, and antibiotic therapy
-
soft tissue
-
evacuate all purulence, debride devitalized tissue, and drill as needed into intraosseous collections
-
send tissue for culture and pathology to rule out neoplasm
-
close wound over drains or pack and return to OR in two to three days
-
-
bone work
-
remove the sequestrum in chronic cases
-
-
-
-
COMPLICATIONS
-
DVT
-
incidence
- is an infrequent complication in children
- is an infrequent complication in children
-
risk factors
-
CRP > 6 mg/dL
-
surgical treatment
-
age > 8-years-old
- MRSA
-
Coagulase (+)
- Causes activation of thrombin and fibrin clot formation
- Causes activation of thrombin and fibrin clot formation
-
-
-
treatment
-
therapeutic anticoagulation
-
-
-
Meningitis
-
Septic arthritis
-
risk factors
- bones with intra-articular metaphysis are at risk (shoulder, elbow, hip, ankle)
-
neonates
- bones with intra-articular metaphysis are at risk (shoulder, elbow, hip, ankle)
-
treatment
-
irrigation and debridement
-
-
- Growth disturbances and limb-length discrepancies from growth plate involvement
-
treatment
-
observation and possible corrective surgery depending on severity or projected severity
-
-
-
Pathologic fractures
-
-
PROGNOSIS
-
Mortality decreased from 50% to <1% with development of antibiotics
-