Summary
-
Juvenile Idiopathic Scoliosis is a coronal plane spinal deformity which most commonly presents in children between ages 4 and 10.
-
Diagnosis is made with full-length standing PA and lateral spine radiographs. MRI studies are indicated in children <10 years old with a curve > 20°.
-
Treatment can be observation, bracing, or surgical management depending on the skeletal maturity of the patient, magnitude of deformity, and curve progression.
Epidemology
-
Incidence
-
15% of all idiopathic scoliosis cases
-
-
Demographics
-
females > males
-
-
Anatomic location
-
most commonly appear as a right main thoracic curve
-
Etiology
-
Associated conditions
-
high incidence of neural axis abnormalities (18-25%)
-
syringomyelia
-
cyst or tubular cavity within spinal cord
-
can be seen in a scoliotic curve without rotation
-
can manifest as an asymmetric umbilicus reflex
-
-
Arnold-Chiari syndrome
-
cerebellar tonsil are elongated and protruding through the opening of the base of the skull and blocking CSF flow)
-
-
tethered cord
-
dysraphism
-
spinal cord tumor
-
-
Classification
-
-
-
-
Early onset scoliosis (EOS)
-
early-onset scoliosis is a broader category including scoliosis in children <10 years old. It includes
-
infantile idiopathic scoliosis
-
juvenile idiopathic scoliosis
-
congenital scoliosis
-
neurogenic scoliosis
-
syndromic scoliosis
-
Marfan's
-
Down's syndrome
-
-
-
-
-
-
Presentation
-
History
-
important to determine when deformity was first noticed and any observed progression
-
get perinatal history
-
-
Presentation
-
failure to develop bowel and bladder control by age ~ 3 or 4 may indicate neurologic involvement
-
patients often referred from school screening where a 7° curve on scoliometer during Adams forward bending test is considered abnormal
-
7° correlates with 20° coronal plane curve
-
-
-
Physical exam
-
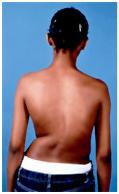
general inspection
-
cafe-au-lait spots (neurofibromatosis)
-
leg length inequality
-
shoulder height differences
-
truncal shift
-
waist asymmetry and pelvic tilt
-
foot deformities (cavovarus)
-
can suggest neural axis abnormalities and warrant a MRI
-
-
-
spine inspection
-
midline skin defects
-
hairy patches
-
dimples (signs of spinal dysraphism)
-
nevi
-
-
rib rotational deformity (rib prominence)
-
Adams forward bending test
-
axial plane deformity indicates structural curve
-
-
forward bending sitting test
-
can eliminate leg length inequality as cause of scoliosis
-
-
-
neurologic
-
motor
-
upper and lower extremities exam
-
-
reflexes
- abnormal abdominal reflexes
-
associated with the presence of a syrinx
-
gently stroking each abdominal quadrant should cause contraction of the abdominal muscles
-
-
clonus
-
Hoffman sign
-
Babinski
- abnormal abdominal reflexes
-
-
gait analysis
-
Imaging
-
Radiographs
-
PA and lateral upright images are used to assess curve severity
-
treatment based on Cobb angle
-
-
Cobb angle
-
> 10° defined as scoliosis
-
intra-interobserver error of 3-5°
-
bending radiographs can help determine which curves require fusion
-
-
- MRI
-
indicated in children <10 years old with a curve > 20°
-
even in the absence of neurologic symptoms
-
must rule out neural axis abnormalities (e.g., syringomyelia)
-
presence of left-sided thoracic curve
-
-
Treatment
-
Nonoperative
-
observation
-
indications
-
curves < 20°
-
-
technique
-
frequent radiographs to observe for curve progression
-
-
-
bracing
-
indications
-
curves 20 - 50°
-
designed to prevent curve progression, not correct the curve
-
relative contraindication to bracing is thoracic hypokyphosis
-
-
technique
-
16-23h/day until skeletal growth completed or surgery indicated
-
-
-
-
Operative
- non-fusion procedures (growing rods, VEPTR)
-
indications
-
curves > 50° in small children with significant growth remaining
-
allows continued spinal growth over unfused segments
-
definitive PSF + ASF performed when the child has grown and is closer skeletal maturity
-
-
- traditional growing rods associated with greater curve correction and truncal height gain than VEPTR constructs
-
-
anterior / posterior spinal fusion
-
indications
-
curves > 50° in younger patients
-
required in order to prevent crankshaft phenomenon
-
-
-
posterior spinal fusion
-
indications
-
curve > 50° in older patients near skeletal maturity
-
remains gold standard for thoracic and double major curves (most cases)
-
-
-
anterior spinal fusion
-
indications
-
curve > 50°
-
best for thoracolumbar and lumbar cases with a normal sagittal profile
-
-
- non-fusion procedures (growing rods, VEPTR)
Complications
-
Crankshaft phenomenon
Prognosis
-
High risk of progression
-
70% require treatment (50% bracing, 50% surgery)
-
-
Very few experience spontaneous resolution
-
Can be fatal if not treated appropriately