SUMMARY
-
Genu Valgum is a normal physiologic process in children which may also be pathologic if associated with skeletal dysplasia, physeal injury, tumors or rickets.
-
Diagnosis is made clinically with presence of progressive genu valgum after the age of 7.
-
Treatment is observation for genu valgum <15 degrees in a child <7 years of age. Surgical management is indicated for severe and progressive genu valum in a child > 7 years of age.
EPIDEMIOLOGY
-
Incidence
-
common but true incidence unknown
-
-
Demographics
-
most common age of presentation 3-5 years
-
range 2-8 yrs
-
-
-
Anatomic location
-
distal femur is the more common location of pathological deformity
-
-
Risk factors
-
prior infection or trauma
-
vitamin D deficiency/rickets
-
obesity
-
skeletal dysplasia
-
lysosomal storage diseases
-
ETIOLOGY
-
Osteology
-
knee
-
normal lateral distal femoral angle (LDFA) = 85-90 degrees
-
normal medial proximal tibia angle (MPTA) = 85-90 degrees
-
hypoplastic lateral femoral condyle with shallow lateral femoral sulcus
-
-
-
Ligament
-
medial collateral ligament
-
2 components
-
superficial
-
femoral attachment medial epicondyle
-
tibial attachment proximal tibia deep and posterior to pes anserinus
-
-
deep MCL
-
composed of meniscofemoral and meniscotibial ligaments
-
-
-
may be attenuated in genu valgum
-
-
-
Tendon
-
increased combined lateral vector of quadricep and patellar tendon (increased q-angle)
-
predispose to patellar instability
-
-
-
Nerves
-
common peroneal nerve
-
branch off sciatic nerve that winds laterally around fibular neck
-
bifurcates into two branches
-
superficial peroneal nerve
-
innervates lateral compartment of leg which controls eversion of foot
-
-
deep peroneal
-
innervates anterior compartment of leg which controls dorsiflexion
-
-
-
-
-
Biomechanics
-
mechanical axis
-
center of femoral head to center of ankle should pass through center of knee
-
lateral deviation of mechanical axis in genu valgum
-
lateral femoral condyle and lateral tibia plateau subjected to increased loads
-
-
-
mechanical loading on physis modulates growth
-
Hueter–Volkmann law
-
compression inhibits growth
-
distraction stimulates growth
-
-
greater proportion of change in growth rate from hypertrophic zone (75%) than proliferative (25%)
-
greater effect on growth seen from change in size of chondrocytes than number
-
-
-
CLASSIFICATION
-
No uniform classification
-
unilateral vs bilateral
-
based on underlying etiology
-
DIFFERENTIAL DIAGNOSIS
-
Physiologic genu valgum must be differentiated from pathologic causes
-
physiologic
-
apparent
-
obesity resulting in large thighs
-
excessive femoral anteversion
-
excessive external tibial torsion
-
-
idiopathic
-
post-traumatic
-
Cozen phenomenon
-
malunion
-
physeal arrest
-
-
metabolic
-
renal osteodystrophy
-
hypophosphatemic rickets
-
-
infection
-
osteomyelitis
-
-
neuromuscular
-
poliomyelitis
-
-
neoplastic
-
multiple hereditary exostoses
-
fibrous dysplasia
-
osteochondromas
-
-
lysosomal storage disease
-
mucopolysaccharidosis type IV (Morquio)
-
-
skeletal dysplasia
-
Chondroectodermal dysplasia (Ellis-van Creveld)
-
Spondyloepiphyseal dysplasia tarda
-
Pseudoachondroplasia
-
Focal Fibrocartilaginous dysplasia
-
-
PRESENTATION
-
History
-
medical and family history can help differentiate between physiological and pathological etiology
-
-
Symptoms
-
cosmetic deformity most common complaint
-
often asymptomatic
-
medial sided knee pain
-
-
Physical exam
-
abnormal circumduction gait
-
inspection
-
hip adduction
-
medial aspect of knees touching
-
wide intermalleolar distance (>8 cm)
-
leg lengths
-
-
range of motion
-
assess patellar tracking
-
-
rotational profile
-
apparent genu valgum with excessive femoral anteversion or external tibial torsion
-
-
general exam to assess stigmata of associated conditions
-
rickets
-
syndromic features
-
skeletal dysplasias
-
Maffucci syndrome
-
-
IMAGING
-
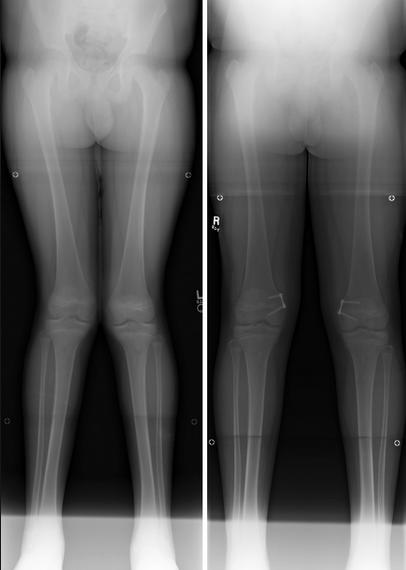
Radiographs
-
indication
-
asymmetrical findings
-
excessive genu valgum clinically age group beyond which is expected of physiologic changes
-
short stature
-
history of trauma or infection
-
limb length discrepancy
-
-
views
-
AP standing long-length film
-
patella should be facing forward to ensure proper positioning
-
-
-
findings
-
lateral deviation of mechanical axis through knee
-
physeal narrowing or premature closing
-
Park-Harris lines
-
-
-
CT or MRI
-
rarely indicated
-
evaluate underlying malignancy
-
evaluate for physeal bar
-
-
STUDIES
-
lab studies
-
depends on suspected underlying medical conditions
-
rickets
-
serum calcium and phosphate
-
25-OH Vit D3 levels
-
PTH
-
-
mucopolysaccharidoses
-
urinalysis for excess muscopolysaccharides (ie keratan sulfate - Morquio)
-
-
syndromic
-
genetic testing
-
-
-
TREATMENT
-
Nonoperative
-
indications
-
first line treatment
-
tibiofemoral angle <15 degrees
-
children <7 years of age
-
-
modalities
-
observation and medical management
-
bracing
-
rarely used
-
-
-
outcomes
-
vast majority of physiological genu valgum will resolve spontaneously
-
medical management of underlying etiology may slow progression
-
bracing may provide temporary relief but is an ineffective long-term solution
-
-
-
Operative
-
indications
-
tibiofemoral angle > 15 degrees
-
intramalleolar distance of 10 cm after age 10 years
-
rapidly progressive deformity after age of 7
-
-
modalities
-
medial hemiepiphysiodesis
-
temporary (more common)
-
permanent
-
-
osteotomy
-
distal femoral osteotomy
-
high tibial osteotomy
-
-
-
outcomes
-
eight-plate hemiepiphysiodesis
-
>95% complete correction for idiopathic
-
80% complete correction for pathological
-
-
rate of correction with hemiepiphysiodesis is variable
-
angular correction of 7 degrees per year at the distal femur
-
angular correction of 5 degrees per year at the proximal tibia
-
-
-
TECHNIQUE
-
Observation
-
techniques
-
observation and reassurance
-
-
- Medial hemiepiphysiodesis
-
indications
-
> 15-20° of valgus in a patient between ages 7-10
-
if line drawn from center of femoral head to center of ankle falls in lateral quadrant of tibial plateau in patient > 10 yrs of age
-
-
options
-
temporary hemiepiphysiodesis
-
rigid stapling
-
percutaneous screw (Metaizeau)
-
tension band plate and screws
-
-
permanent hemiepiphysiodesis
-
modified Phemister technique
-
-
-
technique
-
location of hemiepiphysiodesis dependent on 3 factors
-
amount of remaining growth
-
location of deformity
-
severity of deformity
-
-
place extraperiosteally to avoid physeal injury
-
implant placed midsagittal to avoid sagittal plane deformity
-
one eight-plate or two staples per physis is generally sufficient
-
postop
-
follow patients often to avoid varus overcorrection
-
implant removal
-
remove once mechanical axis passes through center or knee or slightly medial
-
account for rebound medial overgrowth resulting in loss of correction
-
more likely in younger patients
-
-
-
growth begins within 24 months after removal of the tether
-
-
-
complications (~5-10%)
-
screw loosening or failure
-
rebound deformity after removal
-
infection
-
premature physeal closure
-
-
- Osteotomy
-
indications
-
insufficient remaining growth to correct deformity with hemiepiphysiodesis
-
skeletally mature patients
-
non-functional growth plate (ie presence of bar, infection etc)
-
-
options
-
lateral distal femur opening wedge osteotomy
-
pros
-
angular correction can be adjusted to desired correction
-
-
cons
-
requires grafting
-
less stable construct
-
prolonged immobilization to allow graft to heal
-
-
-
medial distal femur closing wedge osteotomy
-
pros
-
stable osteotomy
-
shorter period of immobilization
-
avoid distracting lateral common peroneal nerve
-
-
cons
-
technically demanding to remove precise angular wedge
-
-
-
high tibial osteotomy
-
-
technique
-
determining site of osteotomy
-
dependent on site of deformity
-
assess mLDFA and mPMTA
-
femur most common site of deformity
-
-
-
-
complications
-
nonunion
-
neurovascular complication
-
compartment syndrome
-
hardware failure
-
-
COMPLICATIONS
-
Peroneal nerve injury
-
risk factors
-
opening wedge technique
-
-
prevention
-
perform a peroneal nerve decompression at the time of surgery prior to distraction
-
two potential areas of entrapment
-
fascia of the lateral compartment
-
intermuscular septum separating the anterior and lateral compartments
-
-
-
gradual correction of severe deformities can be done with circular external fixator
-
-
-
Nonunion
-
risk factors
-
opening wedge osteotomy
-
>20 deg deformity
-
-
-
Limb length discrepancy
-
closing wedge osteotomy shortens limb
-
opening wedge osteotomy lengthens limb
-
-
Undercorrection
-
insufficient physeal growth or encroaching maturity
-
-
Overcorrection
-
lost to follow-up (12%)
-
-
Rebound phenomenon
-
incidence
-
56%
-
-
defined as a loss of 5 degrees of correction once the plate is removed
-
risk factors
-
femoral deformity
-
younger age at plate application and removal
-
faster correction rate
-
intentional overcorrection increased risk
-
-
treatment
-
consider slight overcorrection prior to implant removal
-
may not prevent rebound growth but may limit recurrence of deformity
-
-
consider performing growth modulation closer to skeletal maturity for milder deformities
-
-
-
Physeal closure
-
very rare (<1%)
-
prevention
-
place implant extraperiosteally
-
remove implant with 2-3 years after insertion
-
-
PROGNOSIS
-
Idiopathic genu valgum has a better prognosis than pathological etiology with hemiepiphysiodesis
-
higher rate of complete correction
-
faster correction rate
-
fewer complications
-
-
Physiologic genu valgum resolves spontaneous in vast majority by age of 7
-
Deformity after a proximal metaphyseal tibia fracture (Cozen) should be observed as most remodel
-
maximum magnitude of deformity reached approximately 12-18 mo after injury
-
resolve spontaneously within 2-4 years
-
-
Threshold of deformity that leads to future degenerative changes is unknown