-
SUMMARY
-
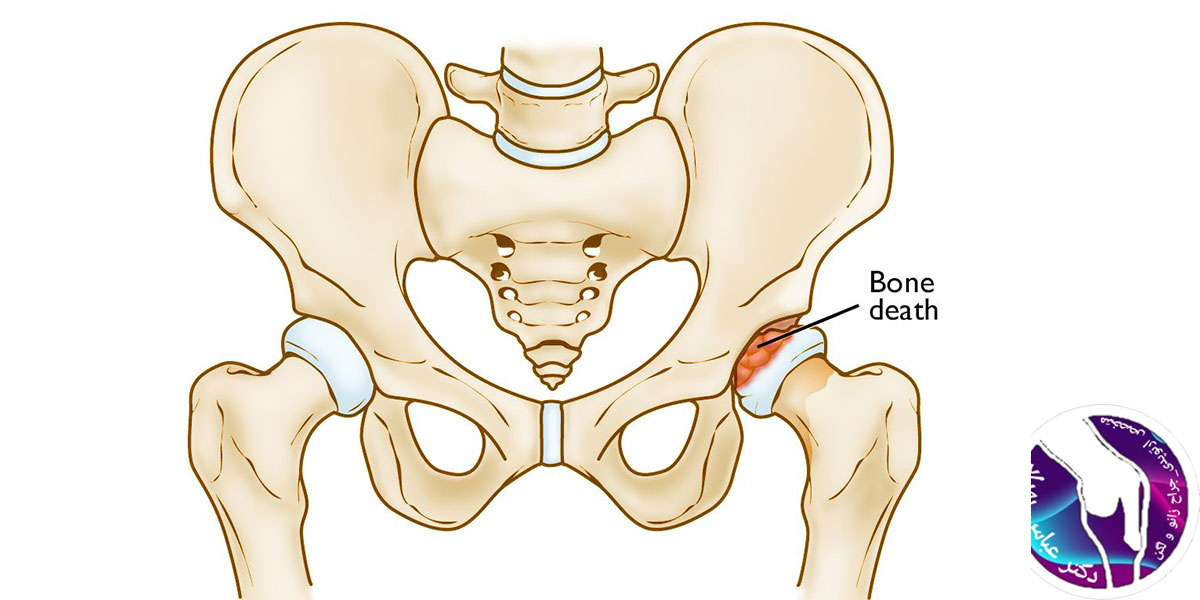
Legg-Calve-Perthes Disease is an idiopathic avascular necrosis of the proximal femoral epiphysis in children.
-
Diagnosis can be suspected with hip radiographs. MRI may be required for diagnosis of occult or early disease.
-
Treatment is typically observation in children less than 8 years of age, and femoral and/or pelvic osteotomy in children greater than 8 years of age.
-
-
EPIDEMIOLOGY
-
Incidence
-
affects 1 in 10,000 children
-
-
Demographics
-
4-8 years is most common age of presentation
-
male to female ratio is 5:1
-
higher incidence in urban areas
-
socioeconomic class
-
higher among lower socioeconomic class
-
-
latitude
-
higher incidence in high latitude (low incidence around equator)
-
-
race
-
Caucasian > East Asian and African American
-
-
-
Anatomic location
-
bilateral in 12%
-
asymmetrical, asynchronous involvement
-
rarely at the same stage of disease
-
-
symmetrical involvement suggests MED (multiple epiphyseal dysplasia)
-
-
-
Risk factors
-
positive family history
-
low birth weight
-
abnormal birth presentation
-
second hand smoke
-
Asian, Inuit, and Central European decent
-
-
-
ETIOLOGY
-
Pathophysiology
-
osteonecrosis occurs secondary to disruption of blood supply to femoral head
-
followed by revascularization with subsequent resorption and later collapse
-
creeping substitution provides pathway for remodeling after collapse
-
-
-
proposed mechanisms
-
possible association with abnormal clotting factors (Protein S and Protein C deficiencies)
-
controversial etiology
-
thrombophilia has been reported to be present in 50% of patients
-
up to 75% of affected patients have some form of coagulopathy
-
-
repeated subclinical trauma and mechanical overload lead to bone collapse and repair (multiple-infarction theory)
-
damages result from epiphyseal bone resorption, collapse, and the effect of subsequent repair during the course of disease
-
-
maternal / passive smoking aggravates
-
-
-
Associated conditions
-
associated with ADHD in 33% of cases
-
bone age is delayed in 89% of patients
-
-
-
CLASSIFICATION
-
Lateral Pillar Classification
-
has best agreement and is most predictive
-
determined during fragmentation stage
- usually occurs 6 months after the onset of symptoms
-
based on the height of the lateral pillar of the capital femoral epiphysis on AP imaging of the pelvis
-
designed to provide prognostic information
-
limitation is that final classification is not possible at initial presentation due to the fact that the patient needs to have entered into the fragmentation stage radiographically
- usually occurs 6 months after the onset of symptoms
-
-
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Waldenstrom classification
-
-
Stages of Legg-Calves-Perthes (Waldenström)
-
Initial
-
Infarction produces a smaller, sclerotic epiphysis with medial joint space widening
-
Radiographs may remain occult for 3 to 6 months
-
Fragmentation
-
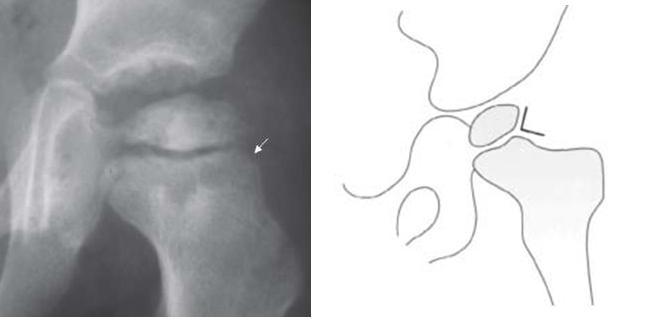
Begins with presence of subchondral lucent line (cresent sign)
-
Femoral head appears to fragment or dissolve
-
Result of revascularization process with bone resorption producing collapse with subsequent patchy density and lucencies
-
Hip related symptoms are most prevalent
-
Lateral pillar classification based on this stage Can last from 6m to 2y
-
Reossification
-
Ossific nucleus undergoes reossification with new bone appearing as necrotic bone is resorbed
-
May last up to 18m
-
Healing or remodeling
-
Femoral head remodels until skeletal maturity
-
Begins once ossific nucleus is completely reossified; trabecular patterns return
-
Catteral Calssification
-
Emphasizes extent of head involvement and outcome (see groups below)
-
Applied during fragmentation stage when the necrotic segment is demarcated from the viable portion
-
Catterall also described head
-
At-risk signs that are associated with poor outcomes
-
Gage sign (V-shaped radiolucency in the lateral portion of the epiphysis and/or adjacent metaphysis)
-
Calcification lateral to the epiphysis
-
Metaphyseal cyst
-
Lateral subluxation of the femoral head
-
Horizontal proximal femoral physis
-
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Salter-Thompson Calssification
|
||
|
|
|
|
|
|
|
|
|
|
-
Stulberg classification
-
Gold standard for rating residual femoral head deformity and joint congruence
-
Recent studies show poor interobserver and intraobserver reliability
-
-
PRESENTATION
-
Symptoms
-
insidious onset
-
may cause painless limp
-
intermittent hip, knee, groin or thigh pain
-
-
Physical exam
-
hip stiffness
-
loss of internal rotation and abduction
-
-
gait disturbance
-
antalgic limp
-
Trendelenburg gait (head collapse leads to decreased tension of abductors)
-
-
limb length discrepancy is a late finding
-
hip adduction contracture can exacerbate the apparent LLD
-
-
-
-
IMAGING
-
Radiographs
-
AP of pelvis and frog leg laterals
-
critical in diagnosis and prognosis
-
-
early findings include
-
medial joint space widening (earliest) from less ossification of head
-
measured between teardrop and ossification center
-
-
irregularity of femoral head ossification
-
decreased size of ossification center
-
sclerotic appearance
-
-
cresent sign (represents a subchondral fracture)
-
-
-
Bone scan
-
can confirm suspected case of LCPD
-
decreased uptake (cold lesion) can predate changes on radiographs
-
-
provides information on extent of femoral head involvement
-
-
MRI
-
early diagnosis revealing alterations in the capital femoral epiphysis and physis
-
more sensitive than radiograph
-
-
Perfusion studies predict maximum extent of lateral pillar involvement
-
Arthrogram
-
a dynamic arthrogram can demonstrate coverage and containment of the femoral head
-
-
-
STUDIES
-
Histology
-
femoral epiphysis and physis exhibit areas of disorganized cartilage with areas of hypercellularity and fibrillation
-
-
-
DIFFERENTIAL
-
Radiographic differential diagnosis
-
infecitious etiology
-
septic arthritis, osteomyelitis, pericapsular pyomyositis
-
-
transient synovitis
-
multiple epiphyseal dysplasia (MED)
-
spondyloepiphyseal dysplasia (SED)
-
sickle cell disease
-
Gaucher disease
-
hypothyroidism
-
Meyers dysplasia
-
-
-
TREATMENT
-
Goals
-
resolution of symptoms
-
NSAIDs, traction, crutches
-
-
restoration of range of motion
-
physical therapy (may exacerbate symptoms), muscle lengthenings, Petrie casting
-
-
containment of hip
-
improve range of motion, bracing, proximal femoral osteotomy, pelvic osteotomy
-
ensure that femoral head is well seated in acetabulum
-
-
-
-
Nonoperative
-
observation alone, activity restriction (non-weightbearing), and physical therapy (ROM exercises)
-
indications
-
children < 8 years of age (bone age <6 years)
-
young patients typically do not benefit from surgery
-
-
lateral pillar A involvement
-
-
technique
-
activity restriction and protected weight-bearing during earlier stages until reossification is complete
-
main goals of treatment are to keep the femoral head contained and maintain good motion
-
containment limits deformity and minimizes loss of sphericity
-
lessen subsequent degenerative changes
-
-
-
bracing and casting for containment have not been found to be beneficial in a large, prospective study
-
all patients require periodic clinical and radiographic followup until completion of disease process
-
-
outcomes
-
good outcomes correlate with a spherical femoral head
-
60% do not require operative intervention
-
good outcomes associated with lateral pillar A and Catterall I groups
-
-
-
-
-
Operative
- femoral and/or pelvic osteotomy
-
indications
-
children > 8 years of age, especially lateral pillar B and B/C
-
-
technique
-
proximal femoral varus osteotomy
-
to provide containment
-
-
pelvic osteotomy
-
Salter or triple innominate osteotomy
-
Shelf arthroplasty may be performed to prevent lateral subluxation and resultant lateral epiphyseal overgrowth
-
-
-
outcomes
-
children with lateral pillar A and those with B under 8 years did well regardless of treatment
- large recent studies show improved outcomes with surgery for lateral pillar B and B/C in children > 8 years (bone age >6 years)
-
studies sugggest earlier surgery before femoral head deformity develops may be best
-
poor outcome for lateral pillar C regardless of treatment
-
-
-
valgus and/or shelf osteotomies
-
indications
- hinge abduction
-
lateral extrusion of the capital femoral epiphysis producing a painful hinge effect on the lateral acetabulum during abduction
-
- hinge abduction
-
abduction-extension osteotomy
-
reposition the hinge segment away from the acetabular margin
-
correct shortening from fixed adduction
-
improve abductor mechanism by improving abductor muscle contractile length
-
-
Shelf or Chiari osteotomies are also considered when the femoral head is no longer containable
-
-
hip arthroscopy
-
emerging treatment modality for mechanical abnormalities in the setting of healed LCPD
-
femoroacetabular impingement
-
-
-
hip arthrodiastasis
-
indications
-
controversial indications and outcomes
-
-
technique
-
hip distraction via external fixation
-
-
- femoral and/or pelvic osteotomy
-
-
TECHNIQUE
-
Proximal Femoral Varus Osteotomy (VRDO)
-
indications
-
extrusion in early stages of LCPD
-
-
technique
-
reposition femoral head into acetabulum for containment purposes
-
-
-
-
COMPLICATIONS
-
Femoral head deformity
-
coxa magna
-
widened femoral head
-
-
coxa plana
-
flattened femoral head
-
-
important prognostic factor
-
Stulberg classification
-
-
-
Lateral hip subluxation (extrusion)
-
associated with poor prognosis
-
can lead to hinge abduction
-
-
-
Premature physeal arrest
-
trochanteric overgrowth
-
coxa breva
-
shortened femoral neck
-
-
leg length discrepancy
-
typically mild
-
-
-
Acetabular dysplasia
-
poor development secondary to deformed femoral head
-
can alter hip congruency
-
-
Labral injury
-
secondary to femoral head deformity
-
femoroacetabular impingement
-
-
-
Osteochondritis dissecans
-
can lead to loose fragments
-
- Degenerative arthritis
-
Stulberg I and most Stulberg II hips perform well for the lifetime of the patient
-
-
-
PROGNOSIS
-
Important prognostic variables
- younger age (bone age) < 6 years at presentation is most important good prognostic indicator
-
sphericity of femoral head and congruency at skeletal maturity (Stulberg classification)
-
lateral pillar classification
- younger age (bone age) < 6 years at presentation is most important good prognostic indicator
-
Variables of poor prognosis
-
female sex
-
decreased hip abduction (adduction contracture)
-
heavy patient
-
longer duration from onset to completion of healing
-
stiffness with progressive loss of ROM
-
Catterall "head at risk" signs (see under classification)
-
-
Natural history
-
long-term studies suggest that most patients do well until fifth or sixth decade of life
-
approximately 1/2 of patients develop premature osteoarthritis secondary to an aspherical femoral head
-
-
Self-limiting process
-
variable course to final healing from initial ischemic event
-
can take 2-5 years to resolve
-
-
Differentiated from adult osteonecrosis by its ability to heal and remodel
-