


-
SUMMARY
-
Radius and ulnar shaft fractures, also known as adult both bone forearm fractures, are common fractures of the forearm caused by either direct trauma or indirect trauma (fall).
-
Diagnosis is made by physical exam and plain orthogonal radiographs.
-
Treatment is generally surgical open reduction and internal fixation with compression plating of both the ulna and radius fractures.
-
-
EPIDEMIOLOGY
-
Demographics
-
highest incidence in
-
men between 10 and 20 years old
-
women over 60 years old
-
-
-
-
ETIOLOGY
-
Pathophysiology
-
mechanism of injury
-
direct trauma
-
direct blow to forearm
-
-
indirect trauma
-
motor vehicle accidents
-
falls from height
-
axial load applied to the forearm through the hand
-
-
sports injuries
-
-
-
-
Associated conditions
-
elbow and DRUJ injuries
-
Galeazzi fractures
-
Monteggia fractures
-
Essex-Lopresti injuries
-
-
compartment syndrome
-
evaluate compartment pressures if concern for compartment syndrome
-
-
-
-
ANATOMY
-
Osteology
-
axis of rotation of forearm runs through radial head (proximal) and ulna fovea (distal)
-
distal radius effectively rotates around the distal ulna in pronosupination
-
-
radial bow accommodates rotation
-
radial bow is complex and not just in coronal or sagittal plane
-
maximal radial bow in the coronal plane is about 15mm at 60% distally along the radius
-
-
the ulna has a slight bow along the distal 75% of the shaft
-
-
Ligaments
-
Interosseous membrane (IOM)
-
occupies the space between the radius and ulna
-
permits rotation of the radius around the ulna
-
connects the radius and ulna obliquely
-
axial load through the forearm begins in the distal radius and then transferred to the proximal ulna
-
distal fibers have the most tension in supination
-
the central fibers are under the most tension in a neutral position
-
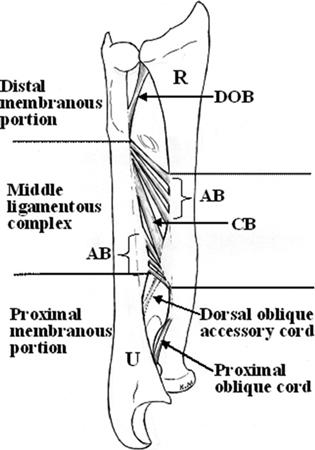
- comprised of 5 ligaments
-
central band is key portion of IOM to be reconstructed
-
accessory band
-
distal oblique bundle
-
proximal oblique cord
-
dorsal oblique accessory cord
-
-
-
-
Nerves
-
median nerve
-
runs with the brachial artery and then courses between the heads of the pronator teres
-
then courses between the FDS and FDP until the carpal tunnel
-
-
ulnar nerve
-
in the forearm, begins between the heads of the FCU
-
then innervates the FDP to the ring and small fingers
-
divides into the motor and sensory branches in the hand
-
-
radial nerve
-
splits into the superficial branch and the PIN
-
the superficial branch runs along the deep fascia to the brachioradialis
-
PIN
-
runs around the radial neck and through the supinator
-
then runs along the posterior interosseous membrane terminating in the wrist capsule beneath the 4th extensor compartment
-
-
-
-
Vasculature
-
the brachial artery branches into the radial and ulnar arteries 1cm past the elbow joint
-
the radial artery is adherent to the FCRL
-
-
-
CLASSIFICATION
-
Anatomic / Descriptive
-
closed versus open
-
location
-
comminuted, segmental, multi-fragmented
-
displacement
-
angulation
-
rotational alignment
-
-
OTA classification
-
radial and ulna diaphyseal fractures
-
Type A (simple)
-
simple fracture that is spiral (A1), oblique (A2), or transverse (A3)
-
-
Type B (wedge)
-
wedge fracture that is intact (B2) or fragmentary (B3)
-
-
Type C (multifragmentary)
-
multifragmentary fracture that is intact segmental (C2) or fragmentary segmental (C3)
-
-
-
-
-
PRESENTATION
-
Symptoms
-
pain and swelling
-
loss of forearm and hand function
-
-
Physical exam
-
inspection
-
gross deformity
-
open injuries
-
check for tense forearm compartments
-
-
vascular
-
assess radial and ulnar pulses
-
-
neuro
-
document median, radial, and ulnar nerve function
-
-
provocative tests
-
pain with passive stretch of fingers
-
alert to impending or present compartment syndrome
-
-
-
-
-
IMAGING
-
Radiographs
-
recommended views
-
AP and lateral views of the forearm
-
-
additional views
-
oblique forearm views for further fracture definition
-
ipsilateral AP and lateral of the wrist and elbow
-
to evaluate for associated fractures or dislocation
-
radial head must be aligned with the capitulum on all views
-
-
-
-
CT
-
indications
-
rarely needed
-
may be helpful for possible occult fractures, evaluating intraarticular extension, or complex fracture characteristics
-
-
-
-
TREATMENT
-
Nonoperative
-
closed reduction and immobilization
-
indications
-
rare
-
completely nondisplaced fractures in patients who are not surgical candidates
-
-
-
techniques
-
bracing
-
functional fracture brace
-
-
casting
-
Muenster cast with good interosseous mold
-
-
-
outcomes
-
loss of >50 degrees of rotation in 30% of patients
-
high rates of non-union associated with non-operative management
-
-
-
-
Operative
-
closed reduction and external fixation (ExFix)
-
indications
-
severe soft tissue injury (Gustilo IIIB)
-
-
-
open reduction internal fixation (ORIF)
-
indications
- nearly all both bone fractures in surgical candidates
- Gustilo I, II, and IIIa open fractures may be treated with primary ORIF
- nearly all both bone fractures in surgical candidates
-
outcomes
-
goal is for cortical opposition, compression, and restoration of forearm anatomy
- most important variable in functional outcome is to restore the radial bow
-
> 95% union rates of simple both bone fractures with compression plating
-
up to 88% union in comminuted fractures treated with bridge plating
-
-
-
open reduction internal fixation (ORIF) + bone grafting
-
indications
-
open fractures with significant bone loss
- bone loss that is segmental or associated with open injury (primary or delayed grafting in open injuries)
-
nonunions of the forearm
-
-
outcomes
-
use of autograft may be critical to achieving fracture union
-
-
-
closed reduction and intramedullary fixation (IMN)
-
indications
-
very poor soft-tissue integrity
-
-
outcomes
-
not preferred due to lack of rotational and axial stability and difficulty maintaining radial bow
-
high nonunion rate
-
IMN does not provide compression across fracture site
-
-
-
-
-
-
TECHNIQUES
-
Closed reduction and immobilization
-
technique
-
functional brace or Muenster cast
-
cast/brace should extend just above elbow to control forearm rotation
-
monitor very closely (~1 week) for displacement
-
should be worn for at least 6 weeks
-
-
-
-
External fixation (ExFix)
-
technique
-
2nd and 3rd metacarpal shafts can both be utilized for distal pin placement
-
pin diameter should not exceed 4 mm
-
-
-
Open reduction internal fixation (ORIF)
-
approach
-
fixation of the fracture with less comminution restores length and may facilitate reduction of other bone
-
typically the radius is fixed first
-
- usually performed through separate approaches due to risk of synostosis
-
radius
-
volar (Henry) approach to radius
- best for distal 1/3 and middle 1/3 radial fractures
- best for distal 1/3 and middle 1/3 radial fractures
-
dorsal (Thompson) approach to radius
-
can be utilized for proximal 1/3 radial fractures
-
-
-
ulna
-
subcutaneous approach to ulna shaft
-
-
-
-
technique
- 3.5 mm DCP plate (AO technique) is standard
-
4.5 plates no longer used due to increased rate of refracture following removal
-
stiff 2.7mm locking plates may be used, but smaller recon plates should not be used
-
-
stainless steel plates provide greater bending rigidity than titanium
-
longer plates are preferred due to high torsional stress in forearm
-
may require contouring of plate
-
-
compression mode preferred to achieve anatomic primary bony healing
-
to minimize strain, six cortices proximal and distal to fracture should be engaged
-
-
locked plates are increasingly indicated over conventional plates in osteoporotic bone
- bridge plating may be used in extensively comminuted fractures
-
interfragmentary lag screws (2.0 or 2.7 screws) if necessary
-
open fractures
-
irrigation and debridement should be performed to remove any contaminated tissue or bony fragments without soft tissue attachments
-
-
plate placement
-
placement of plates on dorsal (tension) side is biomechanically superior but volar placement offers better place seating and soft tissue coverage
-
- 3.5 mm DCP plate (AO technique) is standard
-
postoperative care
-
early ROM unless there is an injury to proximal or distal joint
- should be managed with a period of non-weight bearing due to risk of secondary displacement of the fracture
-
generally 6 weeks
-
-
clinical healing typically occurs at 3 months
-
-
-
Open reduction internal fixation (ORIF) + bone grafting
-
technique
- cancellous autograft is indicated in radial and ulnar fractures with significant bone loss
- vascularized fibula grafts can be used for large defects and have a lower rate of infection
-
Masquelet technique (induced-membrane technique) can also be utilized in cases of non-union or open fractures with significant bone loss
-
2 stage technique
-
1st stage: I&D, cement spacer, and temporizing fixation
-
2nd stage: placement of bone graft into induced membrane and definitive fixation
-
-
- cancellous autograft is indicated in radial and ulnar fractures with significant bone loss
-
-
Closed reduction and intramedullary Fixation (IMN)
-
approach
-
ulnar nail
-
inserted through the posterior olecranon
-
-
radial nail
-
inserted between the extensor tendons near Listers tubercle
-
-
-
technique
-
nails may need to be bent to accommodate for the radial bow
-
may use a small incision at fracture site to facilitate passing of nail
-
-
-
-
COMPLICATIONS
-
Synostosis and Stiffness
-
incidence
-
reported between 3 to 9%
-
-
risk factors
-
associated with ORIF using a single-incision approach
-
-
treatment
- heterotopic bone excision can be performed with low recurrence risk as early as 4-6 months post-injury when prophylactic radiation therapy and/or indomethacin are used postoperatively
- heterotopic bone excision can be performed with low recurrence risk as early as 4-6 months post-injury when prophylactic radiation therapy and/or indomethacin are used postoperatively
-
-
Surgical Site Infection (SSI)
-
incidence
-
3% incidence with ORIF
-
-
risk factors
-
open fractures
-
-
-
Compartment syndrome
-
incidence
-
about 1% overall
-
up to 15% depending on mechanism and fracture characteristics
-
-
risk factors
-
high energy crush injury
-
open fractures
-
low-velocity GSWs
-
vascular injuries
-
coagulopathies (DIC)
-
-
treatment
-
fasciotomy
-
release of the superficial volar compartment alone may be adequate because the compartments are connected
-
other structures that may be released include: the mobile wad fascia, lacerates fibrosus, extensor compartment, deep volar compartment, and carpal tunnel
-
-
-
-
Nonunion
-
incidence
-
< 5% after compression plating
-
up to 12% in extensively comminuted fractures treated with bridge plating
-
-
risk factors
-
extensive comminution
-
poorly applied plate fixation
-
IMN fixation
-
-
treatment
- atrophic nonunions can be treated with 3.5 mm plates and autogenous cancellous bone grafting
-
hypertrophic nonunions can be treated by increasing fixation
- Infection and atrophic nonunions can also be treated with the Masquelet technique
- atrophic nonunions can be treated with 3.5 mm plates and autogenous cancellous bone grafting
-
-
Malunion
-
risk factors
-
direct correlation between restoration of radial bow and functional outcome
-
-
-
Nerve injury
-
risk factors
-
PIN injury with Monteggia fractures and Henry (volar) approach to middle and upper third radial diaphysis
-
median nerve may be injured in the modified Henry approach
-
cutaneous branch of the ulnar nerve is at risk during the approach to the ulna
-
Type III open fractures
-
-
treatment
-
observe for three months to see if nerve function returns
-
explore if no return of function after 3 months
-
-
-
- Refracture
-
incidence
-
up to 10% with early removal
-
-
risk factors
-
removing plate too early
-
plates should not be removed < 1 year from implantation
-
-
large plates (4.5 mm)
-
comminuted fractures
-
persistent radiographic lucency
-
-
treatment
-
wear functional forearm brace for 6 weeks and protect activity for 3 months after plate removal
-
-
-
-
PROGNOSIS
-
Overall, good subjective results, but with expected losses in ROM and strength
-
expected losses
-
reduced strength in grip (25% lost), pronation and supination (30% lost), wrist flexion (16% lost), and wrist extension (37% lost)
-
mild expected reduction (<10 deg) in pronation, supination, wrist flexion, and wrist extension
-
-
- Functional results depend on the restoration of radial bow
-
malunion of the radius and ulna with angulation > 20 degrees is likely to limit forearm rotation
-
-
